Vaginal Prolapse: Causes, Symptoms and Treatment
What Is a Vaginal Prolapse?
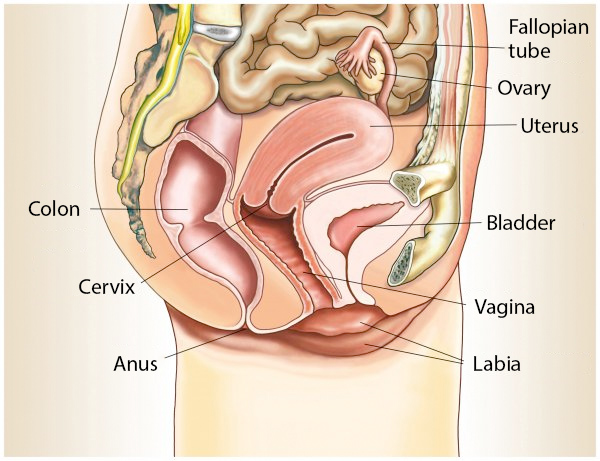
Connective tissue, muscles and ligaments hold the organs of the pelvic floor in place. With age or due to childbirth, connective tissue weaknesses can occur in women. In some cases, this weakness results in organ prolapse.
Approximately 10% of women who have given birth may experience a condition known as vaginal prolapse. The anterior vaginal wall or the posterior vaginal wall can drop and, in particularly severe cases, bulge out of the vaginal entrance. It is also referred to as vaginal prolapse if the patient's uterus has already been removed and the end of the vagina has been stitched up. Vaginal prolapse can be treated conservatively with various physical exercises to strengthen the connective tissue and pelvic muscles. In severe cases and depending on the type of prolapse (e.g. prolapse of the anterior or posterior vaginal wall), various surgical procedures may also be used for treatment.
Our urogynaecology specialists at the Hirslanden Continence Centre in Switzerland provide individual advice to patients and discuss possible treatment methods with them.
Find Out More Now
Contact our specialists for a consultation. We will be happy to inform you about your individual treatment options.
Symptoms and Appearance of Vaginal Prolapse
The symptoms of vaginal prolapse are very similar to those of uterine prolapse or bladder prolapse. Patients usually report the following symptoms:
- a downward pull in the vagina or lower back
- a foreign body sensation inside or outside the vagina
- Bladder symptoms, such as a slow urinary stream, bladder emptying disorder, frequent urge to urinate or increased urge to urinate, incontinence and loss of urine during physical exertion
- Bowel symptoms, such as constipation and defecation disorders or the need to push the vagina upwards to empty the bowel
- Discomfort during sexual intercourse

In some cases of vaginal prolapse, the organ, in this case the end of the vagina, bulges outwards through the vaginal opening. An unpleasant bulge becomes visible to the affected person. At this point at the latest, those affected should contact a gynaecologist or urogynaecologist for clarification and treatment.
Causes and Types of Vaginal Prolapse
Prolapse of the pelvic organs (bladder, uterus, vagina, rectum) is caused by a natural weakness of the connective tissue that can occur in women after childbirth. Vaginal prolapse is preceded by the removal of the uterus: during this operation, the vaginal end is sutured after the organ has been removed. Due to weak pelvic floor muscles and weak connective tissue, the sutured end can sink downwards and out of the vaginal opening.
In addition to childbirth, other causes can also lead to vaginal prolapse. These are:
- Ageing and the menopause lead to an increasing weakening of the pelvic floor
- Overweight
- Chronic cough
- Chronic constipation
- other connective tissue disorders such as Marfan or Ehlers-Danlos syndrome
In addition to prolapse of the vaginal end, other types of vaginal prolapse can also occur. These are the prolapse of the anterior vaginal wall (cystocele) and the prolapse of the posterior vaginal wall (rectocele or enterocele).
What Happens If the Anterior Vaginal Wall Drops?
The prolapse of the anterior vaginal wall, the so-called cystocele, is usually due to the weakness of the strong layer of connective tissue, also known as fascia. This layer on the anterior vaginal wall separates the vagina and bladder. The lowering of the vaginal wall usually causes the bladder to lower as well. This can lead to difficulties urinating with a slow or alternating stream of urine. In most cases, this lowering of the vaginal wall also causes an increased urge to urinate and incontinence.
What Is Posterior Vaginal Wall Prolapse?
A weakness in the connective tissue between the vagina and the lower part of the intestinal tract (rectum) can lead to a posterior vaginal wall prolapse. This form of vaginal prolapse can cause difficulties with bowel movements. The feeling of a foreign body and a pulling or pressure in the vagina are also common. Prolapse of the posterior vaginal wall can also lead to a protrusion out of the vagina. Vaginal prolapse of the posterior vaginal wall is referred to as a rectocele and/or enterocele.
What Tests Are Used to Diagnose Vaginal Prolapse?
In the event of painful symptoms or signs of bulging through the vaginal opening, a urogynecologist or gynecologist should be consulted.
The doctor will first ask you about your medical history, for example whether you have had your uterus removed, whether you have chronic constipation or other causes that may indicate vaginal prolapse . This is followed by an examination of the female reproductive organs and a cough test.
Subsequently, clinical examination and ultrasound examinations provide more precise information as to whether there is a prolapse of an organ in the pelvis. In the case of vaginal prolapse, a urodynamic examination can reveal the effects of the prolapse on bladder and pelvic floor function.
If there are signs of incontinence, it is important to differentiate it from other forms that are not caused by a sagging of the vaginal end.

How to Fix Vaginal Prolapse: Treatment Options
When treating vaginal prolapse, we differentiate between conservative and surgical treatment methods. The specialists in urogynaecology at the Hirslanden Continence Centre diagnose and treat vaginal prolapse individually. Which form of treatment is suitable for you depends on various factors: What symptoms are you experiencing? How severe is the pain? What stage is the vaginal prolapse? Is there already a bulge through the vaginal opening (prolapse) and how severe is it? Of course, other aspects such as age, child planning and state of health are also taken into account and are included in our treatment.
Conservative Therapy
As a rule, a conservative approach is initially chosen for comparatively mild symptoms (mild degree of prolapse, minor incontinence). The following treatments are used in conservative therapy:
- Pelvic floor training
- Pessaries (medical device, usually made of silicone, which is inserted into the vagina)
- Avoidance of lifting heavy loads
While pelvic floor exercises for vaginal prolapse strengthen the weakened muscles around the organs, a pessary is a medical device that provides mechanical support for the pelvic organs. Pessaries come in different sizes and shapes, so we advise our patients on which support is right for them.
Surgical Procedures for Treating Vaginal Prolapse
If the vaginal prolapse is more severe, surgery is also an option. In most cases, surgical intervention is necessary, especially in the final stage of vaginal prolapse, when the vagina protrudes partially or completely from the vaginal opening. A robot-assisted surgical procedure such as DaVinci surgery is also considered by the doctor in cases of severe vaginal prolapse. With this method, the surgeon is assisted by a robot, which transfers the surgeon's movements to the instruments with extreme precision and provides the surgeon with an improved view of the surgical field. This method has the following advantages for the patient:
- Minimal surgical scars
- Low need for painkillers
- Low blood loss
- Faster recovery
- Short hospital stay
Sacrocolpopexy is an operation that corrects a prolapse of the vaginal end after removal of the uterus. The bladder and rectum are first detached from the vagina via an abdominal incision or laparoscopy before a non-dissolvable mesh is sutured to the vagina from the front and back. The mesh is then fixed to the sacrum. Placing the peritoneum over the mesh prevents adhesion to the bowel. Sacrocolpopexy can be performed at the same time as incontinence or other prolapse procedures. The aim of the procedure is to reconstruct the original position of the end of the vagina. This alleviates the symptoms of prolapse. Pain, incontinence and other symptoms are alleviated and normal bladder and bowel function is restored.
Would You Like More Information About Individual Treatment Options?
Please contact us for a consultation; we will be happy to provide you with further information.
